Preliminary results from a national survey reveal how the COVID-19 pandemic has impacted advanced practice registered nurses (APRNs), while findings related to the temporary easing of practice restrictions show little effect on APRN practice. In states with restrictive practice requirements, barriers that impact patient care and access continued to exist despite waivers issued to help combat the pandemic.

The initial results were released this week to coincide with National Nurse Practitioner Week (Nov. 8-14). The survey was conducted by Tennessee nursing leaders from the University of Tennessee Health Science Center College of Nursing, University of Tennessee, Knoxville, and Vanderbilt University.
Investigator Wendy Likes, PhD, DNSc, APRN-BC, FAANP, dean and professor at the UTHSC College of Nursing, said it was important that the study identified barriers to health care during the pandemic. “In spite of the executive order, the majority of the APRNs in Tennessee, for example, were unable to realize the benefits of the additional practice flexibility because of the processes and protocols in place at their practices,” Likes said. “This finding shows that our system’s inflexibility hinders our ability to meet the needs of our community.”
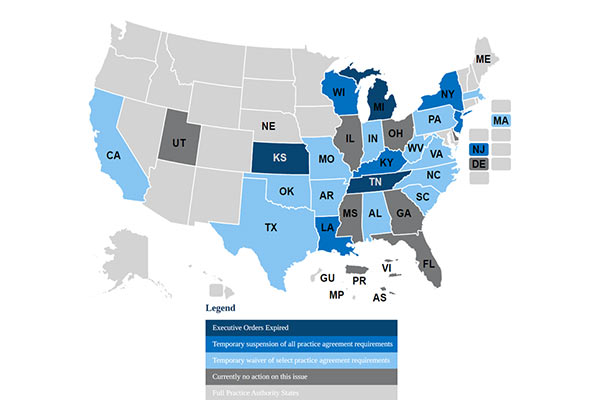
Survey respondents were asked how APRN roles and practices changed during the pandemic, what they saw as ongoing APRN practice barriers, and about the impact of executive orders issued by governors in 21 states with restricted APRN practice that temporarily waived physician oversight of APRNs.

Licensing for APRNs—registered nurses with advanced master’s or doctor of nursing practice degrees—varies from state to state. In 28 states, APRNs practice autonomously without needing physician supervision or oversight.
Some APRNS in states with waivers said that less restrictive executive orders would have allowed them to better meet patients’ health needs. They cited the following barriers: inability to work in another practice area, inability to write orders for home health care or medical equipment, restricted hospital admitting privileges, and the need for physician co-signatures on prescriptions. Some respondents said despite the relaxation of physician oversight, they were still required to pay collaborating physicians.
Investigator Ruth Kleinpell, PhD, RN, FAAN, FAANP, FCCM, Independence Foundation Professor of Nursing Education and associate dean for clinical scholarship at Vanderbilt University School of Nursing, noted that the survey revealed the ways the pandemic changed APRN roles and practices.
“In the early days of the pandemic, some APRNs said they worked in different capacities and roles. Some increased the use of telehealth or were deployed to work in other areas. Some—especially in acute care settings—had an increase in patients, while others saw a decrease in patients and some were even furloughed, especially in primary care settings,” Kleinpell said. “Many APRNS reported playing significant roles meeting the needs of patients, including caring for patients with COVID, coordinating hotlines and managing telehealth services, as well as taking the lead in screening, testing and wellness-based care.”

The investigators emphasized that the full implications of the study are not yet determined. Carole R. Myers, PhD, RN, FAAN, professor at the University of Tennessee, Knoxville, said that it is clear, however, that APRNs have gone to extraordinary lengths to address the health care needs of diverse patients during the crisis. “The foundational knowledge of APRNs and other nurses helped them to deal with problems holistically and be resourceful and creative in finding solutions in difficult and sometimes desperate situations,” she said. “How well APRNs provided services during the pandemic belie the need for outdated supervision requirements and make it hard to justify returning to unneeded practice barriers.”
Mavis Schorn, PhD, CNM, FACNM, FAAN, FNAP, senior associate dean for academics at Vanderbilt University School of Nursing, pointed out that waiving physician oversight resulted in more effective patient care. “While the results are preliminary, it appears that for those APRNs who were able to implement the executive orders, it allowed them to spend more time with patients and less on administrative tasks,” she said. Other benefits included not having to postpone care, being able to follow patients through home health and direct care, and greater efficiency in ordering laboratory tests, medications and durable medical equipment.

The National APRN Practice and Pandemic Survey was conducted June 1–September 23, 2020, with 7,467 APRNs from all 50 states responding. Follow-up interviews were conducted with APRNs in Tennessee as part of a more comprehensive study. The investigators have presented their initial results to the Council for the Advancement of Nursing Science, the American Academy of Nursing and the Tennessee Nurses Association. They continue data analysis and will compare APRN practice in full practice states with those in restricted and reduced states. They will also analyze open-ended comments for themes.
The researchers believe that results support full practice authority for APRNs nationwide, particularly as individual state requirements for collaborative practice and supervision are restricting their ability to provide patient care and limiting patient access to care.
“The pandemic revealed persistent health disparities and major gaps in health care delivery and emergency preparedness,” Myers said. “It is imperative that proven solutions, such as allowing APRNs to practice in all states commensurate with their education and experiences, be deployed to advance equitable access to care for all people. It makes no sense to impose unnecessary barriers when people do not have access to needed care and services.”
Source:
American Association of Nurse Practitioners (AANP) (October 2020). COVID-19 State emergency response: Temporarily suspended and waived practice agreement requirements. Retrieved from: https://www.aanp.org/advocacy/state/covid-19-state-emergency-response-temporarily-suspended-and-waived-practice-agreement-requirements
For more information:
Nancy Wise, APR
Director, Communications
Vanderbilt University School of Nursing
461 21st Ave. S., Rm 117
Nashville, TN 37240
nancy.wise@vanderbilt.edu
t: 615.504.6903
Kara Clark
Coordinator of Community Relations
The University of Tennessee, Knoxville College of Nursing
1200 Volunteer Blvd, Suite 301A
Knoxville, TN 37996
kmclark2@utk.edu
t: 865.974.9498
Leigh Ann Roman
Communications, Marketing and Events Coordinator
The University of Tennessee Health Science Center College of Nursing
920 Madison, Suite 1004
Memphis, TN 38103
lroman2@uthsc.edu
t: 901.448.1561